To the Editor: Closure of the inpatient psychiatric unit at Chelsea Hospital is wrong. Please speak out.
To the Editor:
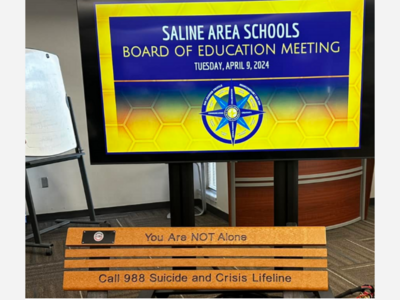
May was Mental Health Awareness month, which highlights the alarming increase in mental illness, including depression, bipolar disorder, schizophrenia, and alcohol and substance use disorders. Patients with acute mental health crises often require inpatient care, but Michigan unfortunately has a shortage of hospital psychiatric beds. There are approximately 29 inpatient psychiatric beds per 100,000 in Michigan, compared to an average of 35 per 100,000 nationally. Clearly, the one thing the state doesn’t need is fewer hospital beds to serve an increasing number of patients with serious mental illness.
Given these statistics, my colleagues and I in the emergency department (ED) at Chelsea Hospital were surprised and dismayed to learn that Trinity Health – which manages Chelsea Hospital - is closing its 30-bed inpatient behavioral health unit later this year. The primary reason for this decision is a shortage of trained mental health professionals, leaving many beds unoccupied despite a demonstrated need for inpatient treatment.
The hospital’s plan for mitigation has three components. First, 12 additional beds will be added to the inpatient psychiatric unit at Trinity Health Ann Arbor (formerly St. Joseph Mercy Hospital). Second, access to outpatient mental health services will be expanded with the goal of preventing the crises that cause patients to need inpatient care. And third, the hospital will be opening a 24/7 holding area for temporarily housing patients with acute mental health conditions until an appropriate facility can be located for their longer-term care. But there are problems with all 3 of these components.
First, Chelsea will replace its 30 beds with only 12 in Ann Arbor, leaving a net loss of 18 throughout Washtenaw County. Fewer overall inpatient beds means that more mental health patients needing hospital admission will be “boarded” in the ED for hours – and often for days - until they can be transferred to another facility that can accept them. And there’s the additional problem of the transfer itself. Because transfer requires an ambulance, and because Huron Valley Ambulance is short-staffed, it can take an additional 12 to 15 hours just to arrange the transfer. In the meantime, these mental health boarders are languishing in the ED without receiving psychiatric treatment. Trinity Health Ann Arbor already has its own ED boarding delays, even worse than Chelsea’s, and ED boarding is in crisis mode throughout Michigan. According to the Michigan Health and Hospital Association, as of May 8 there were 189 ED mental health boarders across the state awaiting inpatient placement.
Third, opening a holding area at Chelsea Hospital will still require adequate staffing by nurses and other mental health professionals, which is the root cause of the low census with the current inpatient unit. ED boarding will persist and likely worsen.
Why is this important to the citizens of Chelsea and surrounding communities who come to the ED with non-mental illness conditions? With more ED beds now occupied by mental health boarders awaiting transfer, it means the next patient who comes to the ED - such as an adult with chest pain or kidney stone, a baby with 103 degree fever, or a pregnant women with vaginal bleeding - will have to wait in the waiting room until an ED bed is available. At Chelsea, with just 3 mental health boarders, our capacity for other ED patients decreases by 15 percent. Clearly, this is not safe.
The solution to psychiatric boarding in the ED is not to close inpatient beds, but rather to increase efforts to recruit and retain qualified mental health professionals to staff them. This can be done by expanding educational opportunities, such as providing scholarships, low-interest college loans or even loan forgiveness for those who choose a career in mental health. It can be done by reducing healthcare worker burnout, by offering flexible work schedules and increasing security measures to prevent patient-directed assaults on staff. And it can be done by increasing the compensation for these highly-desirable professionals. These are the solutions that Trinity Health can and should employ, rather than decreasing the number of inpatient beds which will make the crisis worse.
If you agree that closure of the inpatient psychiatric unit at Chelsea Hospital is wrong, please contact Rob Casalou, president of Trinity Health Michigan, at (734) 712-3792. Tell him that we need to retain this valuable community resource.
James Mitchiner, MD, MPH
Attending Physician
Emergency Department, Chelsea Hospital